Many people experience rectal discharge – whether they have a stoma or not – but if you’re an ostomate, it can be especially surprising. You may have expected that once you had your stoma surgery, nothing more would come out of your bum. So when discharge does occur, it can be worrying.
Anal discharge is a problem that many people feel embarrassed to talk about, so they suffer in silence. Whether it’s a minor inconvenience or something that’s significantly impacting your quality of life, our guide will help you understand why you are experiencing rectal discharge with a colostomy/ileostomy and what you can do about it.
Click to skip directly to a section of the guide:
- Why do I get rectal discharge?
- What is rectal discharge?
- Rectal discharge with mucus
- Rectal discharge with blood
- Rectal discharge with faeces
- Rectal discharge with pus
- What to do about rectal discharge
- How to manage rectal discharge
Why do I get rectal discharge?
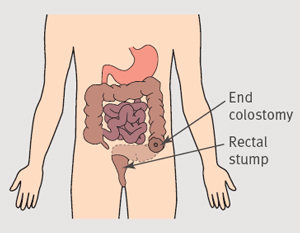
If you’ve had an ileostomy or colostomy, especially following a Hartmann’s procedure or creation of a loop stoma, it’s quite common to experience rectal discharge. This is because a portion of the bowel – known as the rectal stump – is left behind. This part isn’t inactive or “dead”; it still has a blood supply and continues to produce mucus, just as it did before surgery. This is most likely what your anal discharge is made up of, although it may contain other things, which we’ll discuss below.
You might feel pressure in your back passage similar to the urge to have a bowel movement. Some people can wait until they get to a toilet to pass the anal discharge, while others lose sensation post-surgery and may not be able to control it, leading to leakage. Some people even report a persistent feeling that something is stuck in their back passage, which can be very uncomfortable.
What is rectal discharge?
Rectal discharge can consist of:
- Mucus
- Blood
- Faeces
- Pus
We have summarised these in the table below, to help you compare and identify what type of discharge you are experiencing:
| Type of discharge | Appearance | Cause | Medical attention needed? |
| Mucus | Clear, egg-white or yellowish. Liquid, slimy or glue-like. | Natural bodily function | Not typically |
| Blood | Dark to bright red. May appear as streaks in the discharge. | Dark red: Old/dry blood, usually due to healing from surgery. Bright red: Fresh blood, indicates active bleeding in bowel. | Yes if fresh blood |
| Faeces | Discharge may appear brown or have brown spots/streaks. | Loop stoma: High output or diarrhoea. End stoma: Could suggest a fistula. | Inform your stoma nurse |
| Pus | Yellow or green liquid. | Infection | Yes |
Let’s explore this in more detail:
Rectal discharge with mucus
The role of mucus is to lubricate stool as it moves through the bowel, and it’s present in everyone’s digestive system. However, when there is no faeces passing through a part of the bowel, this mucus becomes more noticeable and may cause problems. It can leak out unexpectedly or build up inside the rectal stump, where it may dry out and cause pain or discomfort.
Everyone produces differing amounts of mucus but in general, the more bowel you have remaining, the more mucus your body is likely to produce.
Mucus is usually:
- Clear, egg-white, or yellowish in colour
- Liquid, slimy, or glue-like in consistency
- Sometimes smelly (this is normal)
Rectal discharge with blood
If your rectal discharge is red, this could be a sign of bleeding, but it’s not always a cause for concern. Rectal discharge following stoma surgery may contain dark red blood, which may appear shortly after surgery due to the healing process. This is normal and should reduce over time.
Fresh blood, which appears bright red, could signal active bleeding in the bowel and should be checked by a doctor to determine the cause. It could indicate diversion colitis, a type of inflammation that can develop when the bowel is no longer used for passing stool. Bleeding can also be caused by active inflammatory bowel disease in your remaining bowel. You may need to have an endoscopy and biopsy to diagnose the problem, followed by steroid suppositories or enemas to treat it.
Bleeding in the bowel can also be caused by radiotherapy.

Rectal discharge with faeces
It is possible to pass some faecal matter through your anus even if you have a stoma. This may make your anal discharge appear brown.
If you have a loop stoma, a small amount of faeces can pass into the non-functioning part of your bowel and out through the anus, instead of entering the pouch. This is more likely to occur if you have high output or are experiencing diarrhoea. This is generally not harmful.
If you pass stool from your back passage with an end stoma, it could indicate a fistula between the bowel and rectal stump. Tell your stoma nurse if this happens.
Rectal discharge with pus
Pus is a yellow or green liquid, which may be accompanied with pain. You should speak to your doctor if you think your rectal discharge has pus because it can be a sign of infection.
What to do about rectal discharge
Some people experience rectal discharge every day; others only occasionally, or not at all. Over time, the amount may reduce, but it doesn’t always go away completely. This is because mucus production is a normal function of the bowel. If it isn’t causing major issues, you should be able to adapt and live with your rectal discharge. There are ways to manage it which we will discuss below.
The only way to eliminate it entirely would be to have a proctectomy (commonly referred to as “Barbie butt surgery”) – a procedure where the rectum and anus are surgically removed and the area is closed up. This may be offered to people experiencing persistent or severe issues with rectal discharge like diversion colitis, but it’s not suitable for everyone. Read more in our full article on Barbie Butt Surgery
How to manage rectal discharge
These are our top tips for managing rectal discharge day-to-day:
1. Routine toileting
- If you feel the urge similar to needing a poo, sit on the toilet as if you were going to poo and gently bear down (don’t strain). This should pass any discharge.
- Doing this once a day, even if you don’t feel the urge to go, can help the mucus pass more easily and prevent painful buildup.
2. Suppositories or enemas
- Some people are unable to pass mucus due to a lack of sensation after stoma surgery. If this is the case, suppositories or enemas may help to flush the discharge out.
- Some are available over the counter, but it’s best to speak to your GP or stoma nurse first.
3. Protect your skin
- If the discharge leaks out and you can’t control it (this is particularly common after radiotherapy), this can lead to painful skin damage.
- Use barrier films like StoCare Protect to protect the skin from irritants and reapply after washing.
- Shower regularly or use wet wipes to gently clean the area (avoid scrubbing and alcohol-based products).

4. Use pads
- Thin panty liners or incontinence pads can protect your clothes from any leakage.
- Close-fitting underwear helps to hold pads in place.
5. Pelvic floor exercises
- You can practice pelvic floor exercises to strengthen your sphincter muscles and have better control over discharge from the rectum.
- Ask your stoma nurse for guidance. There are some examples in this NHS article.
Conclusion
Rectal discharge after stoma surgery is normal, although it can be uncomfortable or distressing. If you’re concerned about your rectal discharge, reach out to your doctor or stoma nurse. You don’t need to struggle in silence.
You can also connect with stoma charities, online support groups and fellow ostomates for shared tips and reassurance. The organisations below provide stoma helplines, one-to-one support, support groups and events, private social media pages, information and much more:
- Colostomy UK – including a 24-hour stoma helpline (for anyone with any type of stoma)
- Ileostomy and Internal Pouch Association
- Urostomy Association
- Bladder and Bowel UK
- Bladder and Bowel Community
Although all our articles are written alongside qualified medical professionals, this information is for guidance only and does not replace advice given by your healthcare advisors.



